

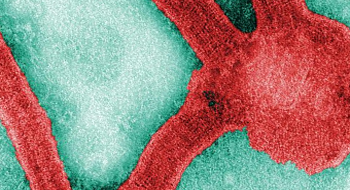

Marburg and Ebola are small viruses in the filovirus family, which contain a 7-gene single-stranded RNA genome. Infection with the only known strain of Marburg virus, Lake Victoria marburgvirus, or the Zaire and Sudan ebolavirus, can cause a deadly viral hemorrhagic fever with a fatality rate ranging from 23-90. Two additional strains of Ebola, the Reston and Ivory Coast ebolavirus, are not deadly to humans. Although filovirus infections can be deadly, human outbreaks are relatively rare and have been located in, or traced to, Africa. Less than 2,000 people have died from filovirus hemorrhagic fevers since the viruses were discovered in the late 60s and 70s. Humans are not a natural part of the filovirus lifecycle and their natural reservoir (host animal) is unknown; however, bats are suspected. Once an individual is infected, the virus spreads to others through direct contact with infected fluids and tissues. Aerosol spread is not likely, but cannot be ruled out.
The Marburg and Ebola viruses are considered effective bioweapon agents for a number of reasons. They can be aerosolized, produced in large industrial quantities and spread from person-to-person. In addition, they have a high fatality rate, a low infectious dose, no known effective vaccine or treatment, and would cause public and healthcare worker panic. The Soviet Union’s biological weapons program favored Marburg over Ebola, and manufactured ton quantities of the Marburg virus after finding its weaponized form to be more stable than Ebola.
The virulence factors and their exact functions are largely unknown in filoviruses and are currently under investigation. Filoviruses can infect and alter or kill a variety of different types of cells. In particular, filoviruses infect the cells of the immune system, which fights infections, the liver, which produces the coagulation proteins in the blood, and the adrenal gland, which has a role in controlling blood pressure. The resulting hemorrhagic fever causes three major problems: 1) Blood clots form in the circulatory system and can cause multi-organ failure. 2) Blood vessels weaken and become permeable, causing bleeding (hemorrhaging) and swelling (edema). 3) The immune system is altered. Some functions are suppressed, such as the antiviral response (Type I IFN), which is likely blocked by two viral proteins (VP35 & VP24), and other functions are over activated, e.g. the inflammatory response. Massive amounts of inflammatory molecules are released by the altered immune cells. These molecules increase the permeability of blood vessels, causing some immune cells to apoptose, or self-destruct, and can send the body into shock.
The non-infectious incubation period can range from 2-21 days, followed by an abrupt onset of a high fever, malaise, headache, prostration, abdominal pain and non-bloody diarrhea. 50% of patients develop a rash similar to measles. Coagulation problems lead to both excessive hemorrhaging (bleeding), and blood clotting throughout the body. The excessive hemorrhaging can be seen as bloodshot eyes, petechiae (blood spots under the skin) and/or bloody urine. Abnormal blood clotting can also cause disseminated intravascular coagulation, a condition where blood clots clog blood vessels throughout the body and damage organs by depriving them of oxygen. Patients may be delirious, have convulsions or fall comatose and typically die 1-2 weeks after symptoms develop from massive bleeding, shock and multi-organ failure. If they recover, patients can remain infectious for approximately 3 months. The Marburg and Ebola viruses have been isolated in seminal fluid over 80 days from disease onset and this route has been implicated in disease transmission.
There are no treatments that specifically address filovirus infection; supportive measures are taken to mitigate the effects of symptoms. IVs and other invasive procedures should be avoided because a patient’s blood may not clot, leading to hemorrhage. Air transport should also be avoided because in-flight air pressure changes can cause damage to blood vessels in the patient’s lungs. Secondary infections are common. Passive immunization, the injection of blood serum from recovering patients (containing antibodies against the virus) has been employed, but its efficacy is unknown and as a treatment, the antiserum would be in limited supply. A preliminary 2003 study with an anticoagulant and anti-inflammatory drug, rNAPc2 (recombinant Nematode Anticoagulant Protein c2), was shown to reduce the mortality of monkeys infected with Ebola virus. It may be a promising treatment in the future.
There are currently no vaccines for filoviruses. Vaccine development has been difficult, and many different development methods have been tried. A vaccine made from a common virus, the adenovirus, which has been altered to produce the Ebola glycoprotein (GP), currently shows promise.
Dembek, Z.F. [Senior Editor] (2007). Viral Hemorrhagic Fevers, Chapter 13, Medical Aspects of Chemical and Biological Warfare. Publisher: Department of Defense, Office of The Surgeon General, US Army, Borden Institute. 2007: 672 p.; ill http://www.bordeninstitute.army.mil/published_volumes/biological_warfare/biological.html
Borio, L. et al. (2002). Hemorrhagic Fever Viruses as Biological Weapons. JAMA, vol 287, No. 18.
Feldman, H., et al. (2003). Ebola virus: from discovery to vaccine. Nature Reviews, Immunology, Vol 3.
Centers for Disease Control, USA (2010). Known Cases and Outbreaks of Ebola Hemorrhagic Fever, in Chronological Order. Accessed 06 May 2010 from http://www.cdc.gov/ncidod/dvrd/spb/mnpages/dispages/ebola/ebolatable.htm
Anon. (2004) Ebola, lab accident death - Russia (Siberia), ProMED-mail 2004; 22 May 2004: 20040522.1377. Accessed 06 May 2010 from http://www.promedmail.org/pls/apex/f?p=2400:1202:2506065928361401::NO::F2400_P1202_CHECK_DISPLAY,F2400_P1202_PUB_MAIL_ID:X,26482
Alibek K. (1999) Biohazard: The Chilling True Story of the Largest Covert Biological Weapons Program in the World—Told from the Inside by the Man Who Ran It. New York, NY: Random House; 1999.
Centers for Disease Control, USA (2009). Imported Case of Marburg Hemorrhagic Fever --- Colorado, 2008. Accessed 06 May 2010 from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5849a2.htm